Dr Andrea Doyle: RCSI Research Profile
23/08/2023
Dr Andrea Doyle’s career to date demonstrates the value of combining research fields to establish new educational standards in medical practice. With a background in medical physics from Technological University Dublin, she has established herself in the field of medical education in RCSI through her work in simulation, ensuring that others can learn from her expertise in medical physics and engineering.
She also focuses on the huge impact her supervisors and mentors have had on her career, including her first PhD supervisor, Prof Browne, who is “one of the people that's had the biggest impact in my professional life, watching what she achieves. She has set me up for success, not just in my research activities, but in my professional development.” When Prof Browne left Ireland for the Mayo Clinic she continued to support Doyle, and they have maintained a working relationship since then. She also worked with Prof Frank Sullivan an oncologist that was involved in the introduction of prostate brachytherapy in Ireland. “He verified and validated the materials and the device I had been working on, because he has experience in thousands of procedures, he knew how it should feel, and he knew how it should respond and how it should look.”
This work led to a patent for their tissue mimicking materials, and since then the team has been in talks to work with industry: just last month, they signed a material transfer agreement between RCSI, Doyle and her small group of colleagues, and an industry partner. Currently, they’re sending samples over to the company who may buy the IP. This would be fantastic, she notes. From the very beginning, they took patient data anonymously for 3D printing, and ensured everything was up to clinical standard. “I think all of that has brought us to the commercialisation point, because we really tried to make a product that somebody would want. Everything was done in a way that would lead to opportunities for success.”
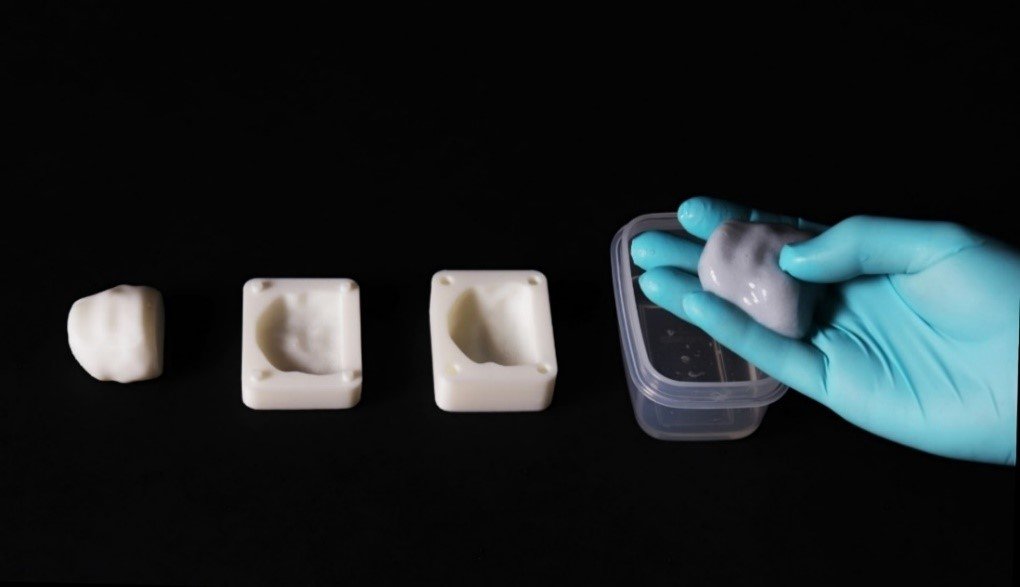
- Anatomically correct prostate target development
Going forward, Doyle’s plan is to assess the landscape of point of care ultrasound education on an international level, to explore how it can be built upon in an Irish setting: UCLA is now integrating ultrasound education into its medical education. Until now it’s been a separate speciality, but ultrasound is becoming an increasingly important field in the radiology department, especially due to recent innovations in technology. She is part of a team hoping to integrate ultrasound education into undergraduate medical degree at RCSI. Dr Doyle is currently applying for funding to go to UCLA, to collaborate and research their methods, and bring back a package of curriculum and assessment to Ireland and Europe.
When it comes to education, she advises students to be inquisitive: “putting your hand up, putting yourself forward, this is how you'll find a mentor. We're moving into an age of education where our teachers are not oracles, they do not have every answer. What we can do is show our students how to become problem solvers. I think that's ultimately what education helps us to do. Putting your hand up, having that bit of confidence in yourself means you can find your tribe, the people you could learn from.”
Her PhD research focused on brachytherapy, a form of radiotherapy that treats prostate cancer. Brachytherapy can be extremely effective, she explains, but if the radioactive material is accidentally placed in the wrong area of the body – somewhere other than the site requiring treatment, such as the bladder – there can be disastrous consequences for patients. While they initially wanted to assess the equipment to ensure it was functioning effectively, Doyle and her team soon realised that there was also a significant need for ultrasound training for health professionals that utilise the equipment. This led them to take a two-pronged approach: to establish both a quality assurance programme, which focused on the ultrasound systems used in brachytherapy, as well as a training programme for health professionals such as oncologists and medical physicists, to ensure they were confident and competent in the procedure.
- Kidney model
This project led Doyle to medical education, as she began lecturing and, once she completed her PhD in 2019, she joined HPEC, RCSI’s Health Professional Educational Centre as a research officer. The 9 months she worked there were “like an apprenticeship in medical education. So much was happening so quickly in medical education due to the COVID pandemic, and so many things had to be changed, I got involved in everything I could.” She also began working with BEME, the Best Evidence Medical Education Collaboration, contributing to two major reviews which were direct responses to the COVID pandemic.
Following this, she took the opportunity to move to RCSI SIM. This, she notes, was “a logical next step to continue down the medical education route” as she introduced training devices to her teaching and contributed to a simulation based communication skills course for child safeguarding: an inter-professional, inter-agency course attended by nurses, doctors, social workers, guards and lawyers among others. “Working with a team led by Prof Walter Eppich, Chair of RCSI SIM, we designed the course and ran it twice. We used the process of design based research which facilitates iterative refinement: you do it, learn from it, and then implement it again, until satisfied. We got wonderful feedback from the health professionals who attended the course letting us know that they’ve changed their practice, and have a greater understanding of their roles and the roles of other professionals as a result of the course.”
In 2021 Doyle began an IRC fellowship, working on an interventional radiology programme, with Prof Eppich, and Dr Claire Condron, Director Education at RCSI SIM, peof Colin Cantwell Consultsnt Interventional Radiologist, St Vincent's Hospital, and Prof Richard Arnett, Director of Psychometrics RCSI. This position came with many challenges because at the time there was no structure to interventional radiology training for graduate radiologists. She therefore began to design mastery-based learning curriculum through simulation. “The goal of the course is that everybody will reach competency,” she explains, “it just requires a bit more time for some versus others on different clinical competencies. This allows people to achieve mastery of these skills. The time it takes to achieve the standard is different for everyone.” Concurrently, she explored the wider landscape of interventional radiology, running a consensus study around the country to ascertain what key competencies should be focused on, and conducting cognitive task analyses to see radiology practices carried out as opposed to simply being theoretical discussions.
During all this time, what has Doyle’s experience of RCSI been like? Describing the “phenomenal centre” she works in, what becomes clear is the interdisciplinary and innovative nature of the work being conducted there. She describes a support atmosphere for all the department team members to be engaged in research “the line has started to blur between operations and research, and a lot of our technicians are getting more involved in structured research projects and programs.” The people she works with include people with backgrounds in technical equipment such as audio/visuals, as they often film simulated medical scenarios so students can reflect on what they see to consolidate their learning. There are technicians working in special effects and makeup for scars and injuries, and simulated participants who attend the training workshops to act out scenarios as patients. She highlights the necessity of enjoying your working environment: “that's where innovation and creativity come from.”
Indeed, Doyle’s own research has required a high degree of interdisciplinarity: when working with her supervisor Dr Jacinta Browne (Mayo Clinic), they started developing material for a training device that would feel like real tissue, as often materials used in training devices do not image well under ultrasound. Doyle’s personal project was to investigate how to make different types of tissue. She highlights the collaboration with the arts and humanities that made this process possible: “I worked with John Walsh the head of TU Dublin’s School Art and Design, and their work was nominated for a “Research and Education” design award from the Institute of Designers in Ireland. It was lovely to see our research from a different point of view, because I was so used to looking at it as science and education.”
Doyle stresses the importance of collaboration in her work: “my question starting a new piece of work is, who are we working with? In our child safeguarding course, we had an emergency medicine paediatric consultant, a paramedic firefighter, and an ex-primary school teacher, all involved in a co-design process. What I'm learning is, often in science we try find a solution to a problem through siloed experimental research. But a lot of the time, it’s the people that are affected by the problem, and the people that are directly facing the problem, that have the answer.”
Dr Andrea Doyle
Dr Andrea Doyle is a medical physicist and postdoctoral researcher at the SIM Centre for Simulation Education and Research at RCSI University of Medicine and Health Sciences, Dublin. She served as a member of the BEME board in 2020. She has also supported staff involved in systematic reviews and educational research as a member of the RCSI BICC in 2020. Her research and training in medical physics and healthcare technology has equipped her to work collaboratively with health professionals in multi-disciplinary teams through the development of anthropomorphic physical simulation devices.
You can follow her on @AndreaJaneDoyle